May is Stroke Awareness Month. Are You Stroke Aware?

Each year, about 800,000 people in the U.S. suffer a stroke. A stroke can cause brain damage, major disability or even death.
What causes a stroke? How can you prevent a stroke? What are the symptoms or warning signs? And what are the treatments? Understanding the answers to these questions could potentially save your life or the life of a loved one.
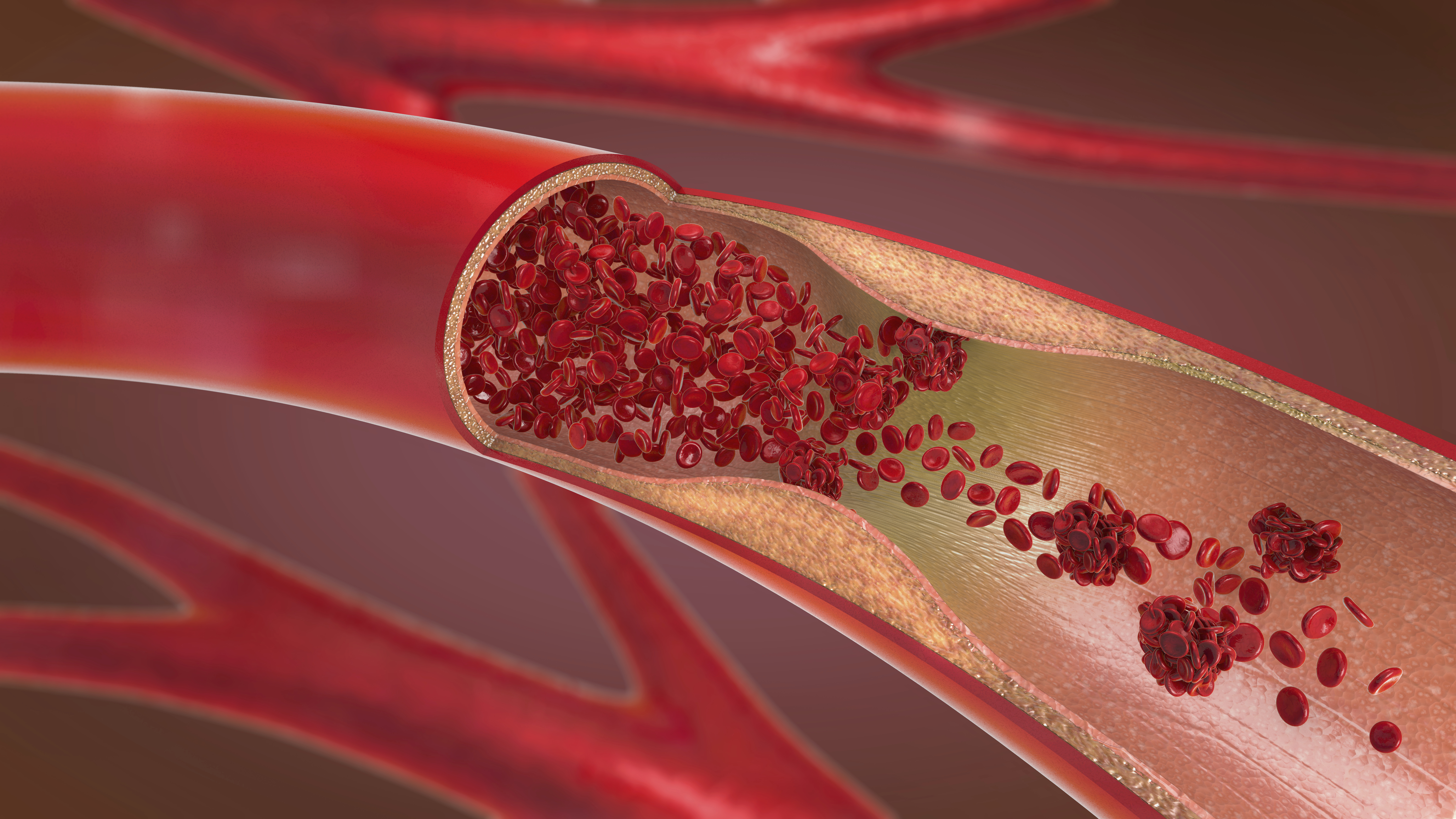
A stroke occurs when there's a sudden loss of blood supply and oxygen to an area of the brain, either due to a blockage of a blood vessel supplying blood to the brain or a rupture of a blood vessel in the brain. Either way, brain cells start to die within minutes.
Symptoms of Stroke-BE FAST!
Symptoms of a stroke vary depending on the type of stroke and what part of the brain is damaged. The signs and symptoms of stroke can easily be remembered with the acronym "BE FAST," which includes sudden changes in balance or ability to walk, blurred vision, brief blindness or double vision, drooping of the face or weakness on one side of the body, difficulty holding your arm up or numbness in one arm, difficulty speaking, difficulty understanding or slurring of words. If you believe you or someone else is having a stroke, call 911 immediately and tell the 911 operator you believe the person is having a stroke.
Understanding Carotid Artery Disease
Most strokes are caused by blockages, often the result of carotid artery disease. Taylor Hicks, MD, assistant professor at McGovern Medical School at UTHealth Houston and vascular surgeon affiliated with Memorial Hermann, explains what causes carotid artery disease, what you can do to prevent it and how it is treated.
"Carotid artery disease is characterized by atherosclerosis-the build-up of atherosclerotic plaque-in the carotid arteries in the neck," says Dr. Hicks. "This plaque can build up on the inside walls of the artery causing stenosis, or narrowing, of the artery. If the plaque ruptures, it can break off and travel to the brain. At site of the rupture, a surface is created where blood clots can form. In turn, those blood clots can be sent to the brain as well, causing worsening strokes."
Prevention is key.
When it comes to strokes, the best "cure" is prevention. As Dr. Hicks explains, while genetics can play a role in your risk of developing atherosclerosis, there are things you can do to significantly lower your risk. "Smoking plays a big role, as well uncontrolled high blood pressure, diabetes and cholesterol," he says.
How would you know you've got carotid artery disease? What are the symptoms? How is it diagnosed?
"Carotid artery disease is typically silent, showing no symptoms," says Dr. Hicks. "Sometimes, during a routine exam, a physician might detect through a stethoscope turbulent blood flow in the carotid artery, an indicator of stenosis. Some diagnoses occur as a result of routine screening via ultrasound, especially among high-risk patients. But most diagnoses occur when a person seeks emergent care for a stroke or a transient ischemic attack (TIA), often called a 'mini-stroke.'"
Multiple Treatments Available
Treatments for carotid artery disease, which include medical management and surgical procedures, depend on the degree of the stenosis and the patient's medical history, says Dr. Hicks. "We typically treat patients who are asymptomatic, meaning those who have not had a TIA or stroke, medically, with low-dose aspirin and statin drugs," he explains. "But surgery is typically recommended for patients whose stenosis is greater than 70%, or greater than 50% in patients who have suffered a stroke, as their likelihood of suffering another stroke is greater."
Vascular surgeons affiliated with Memorial Hermann are skilled at performing all types of surgical procedures to treat carotid artery disease.
"The gold standard of treatment for patients continues to be carotid endarterectomy, a procedure in which the surgeon accesses the artery through an incision in the side of the neck, opens the artery, removes the plaque and repairs the artery," says Dr. Hicks. "We also routinely perform carotid artery angioplasty with stenting, a minimally invasive procedure that widens the narrowed artery by compressing the plaque and using a mesh tube, or stent, to permanently prop the artery open. The artery is accessed by threading a small tube, called a catheter, though a small puncture in the patient's groin."
Vascular surgeons at Memorial Hermann also routinely perform transcarotid artery revascularization, or TCAR, a hybrid approach to carotid stenting which minimizes the risk of stroke during the procedure. "In TCAR, we make a small incision in the base of the neck to access the carotid artery. Blood flow is temporarily reversed during the procedure so that any small bits of plaque that may break off are diverted away from the brain, preventing a stroke from happening. A stent is then placed inside the artery to stabilize the plaque, minimizing the risk of a future stroke," he says.
Patients who undergo the TCAR procedure recover more quickly with less pain, smaller scars and a reduced risk of future strokes when compared to more traditional options.
"The right treatment for a given patient will depend on a number of factors'" says Dr. Hicks. "The surgeon will evaluate the patient and recommend what's best for the patient," he says.
For more information on cardiovascular disease and treatments, or to schedule an appointment with an affiliated heart and vascular specialist, visit memorialhermann.org/heart