Data analysis finds COVID-19 testing lacking in many minority communities

HOUSTON, Texas (KTRK) -- The streets on Houston's southwest side have been a little quieter since COVID-19 hit.
More than two weeks into the city's push to target the surge of positive cases in Houston's Hispanic community, and with no health officials in sight, Gulfton Super Neighborhood Council president Sandra Rodriguez is socially distancing as she listens attentively to residents in the shadow of one of the neighborhood's murals celebrating the community's diversity.
A Spanish-speaking man tells her he was let go from his job at a restaurant and is in need of work. He also tells her he waited over two weeks to get the results of a COVID-19 test.
Frustrated, the man asked Rodriguez, "What's the point?"
In the predominantly Hispanic community, where several generations often live together in crowded apartment buildings and work essential jobs, Rodriguez admits preventing the virus' spread and accessibility to testing is essential. Although a test doesn't stop the virus, a positive result can get people the help they need quicker, before it turns fatal.
The Gulfton neighborhood's 77081 area code has seen at least 12 COVID-19 deaths since the beginning of the pandemic.
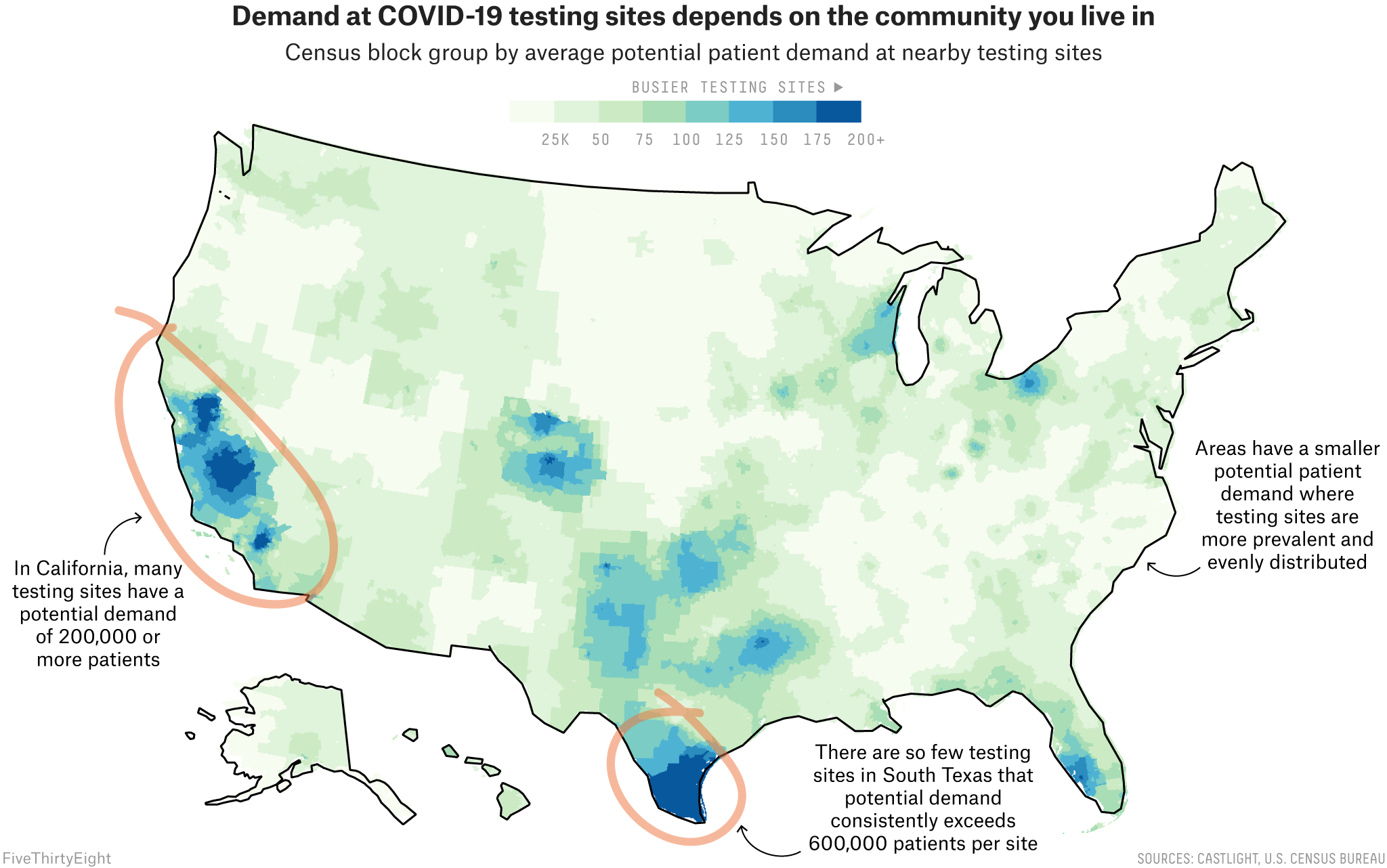
With nearly 4 million coronavirus cases across the United States and hospitalizations surging in different parts of the country, there continues to be a growing demand for tests. Today, Americans routinely wait for hours to get an exam - if they can get one at all. Access is not available equally nationwide. Simply put, where Americans live and how much income they earn can still determine the ease with which they get a COVID-19 test.
According to a new, extensive review of testing sites by FiveThirtyEight, ABC News, and ABC-owned television stations, sites in communities of color in many major cities face higher demand than sites in whiter or wealthier areas in those same cities. The result of this disparity is clear: People of color, especially Black and Hispanic people, are more likely to experience longer wait times and understaffed testing centers.
This nationwide review is one of the first to look at testing site locations coast to coast, in all 50 states plus Washington, D.C., using data provided by the health care navigation company Castlight Health (the same data that Google Maps uses to surface COVID-19 testing sites). An assessment of city and state health department websites also revealed, over and over, fewer testing sites in areas primarily inhabited by racial minorities.
Importantly, the analysis does not factor in the capacity of testing sites, which can vary from just 50 tests at one site to 2,000 at another, meaning that one site might be equipped to serve a larger number of people than another site. Instead, it looks at the potential demand for each site based on the number of people and sites nearby. The data we used is also less likely to reflect tests done in private physicians' offices than federally-funded community sites, local government-run mobile pop-up sites, urgent care clinics and hospitals. Additionally, this analysis doesn't take into account other factors that could determine testing accessibility, such as staffing and wait times, as well as other restrictions on testing like appointment or insurance requirements.
In Texas, there have been 3 million COVID-19 tests statewide as of July 22. Rodriguez, a lifelong Gulfton resident, said accessibility to those tests is an issue for some.
"What about the ones who don't have transportation? What about the ones that are working? They cannot access this location Monday through Friday," Rodriguez said. "We need to provide these services on the weekends, on Saturdays and Sundays when the community is available."
With the exception of a regular testing site at the Southwest Multi Service Center, Gulfton is a sort of testing desert. There are more sites in neighboring Alief and Bellaire, if you can get there -and get there before they close.
"Nine to five?" Rodriguez said. "Those are working hours and many of them are working, but until six or seven."
The number of COVID-19 testing sites changes every day, with the announcement of a neighborhood pop-up site every so often, like the one held by District J city councilman Edward Pollard just this past weekend. Though, after the weekend, the testing site was gone.
Rodriguez says city leaders need to focus on giving underserved communities easy access to nearby testing sites with flexible hours and no questions asked about legal status.
To fight the virus in Hispanic communities, the city of Houston's "Better Together" or "Todos Juntos, Mejor" emergency outreach plan relies in part on social media influencers to get the word out on where to get tested and how to prevent the spread of the virus.
However, Rodriguez said with some minorities busy with a job, or two or three, the city's outreach efforts aren't helping.
"I have to buy groceries, I have to wash my clothes and I come home, those are the point locations where marketing needs to be targeted," she said. "Meeting the community where they are."
The Department of Health and Human Services recently released a comprehensive strategy to address the disparate access to COVID-19 testing, including expanding testing at federally qualified health centers as well as supporting public-private partnerships that establish testing at retail pharmacy companies to accelerate testing within vulnerable populations. CVS and Walgreens - two of the retail pharmacies listed in the HHS plan - both said in statements to ABC News that more than half of their store locations issuing COVID-19 tests are now located in areas most in need, based on the Centers for Disease Control and Prevention's social vulnerability index.
For now, Rodriguez is focused on a project with an immediate impact: helping to organize small groups of neighbors, many out of work, paying them to sew face masks that have been distributed to other Gulfton residents.
"This is something that the community has created, has worked on and now we're giving it back to the community," said Rodriguez.
Sewing masks in living rooms, educating neighbors on the street. It could be the simplest way to keep Gulfton from adding another COVID-19 fatality to its tally.
What our analysis found
The novel coronavirus itself does not distinguish between Black and white Americans. But virtually every other aspect of U.S. society does, including the nation's response to COVID-19.
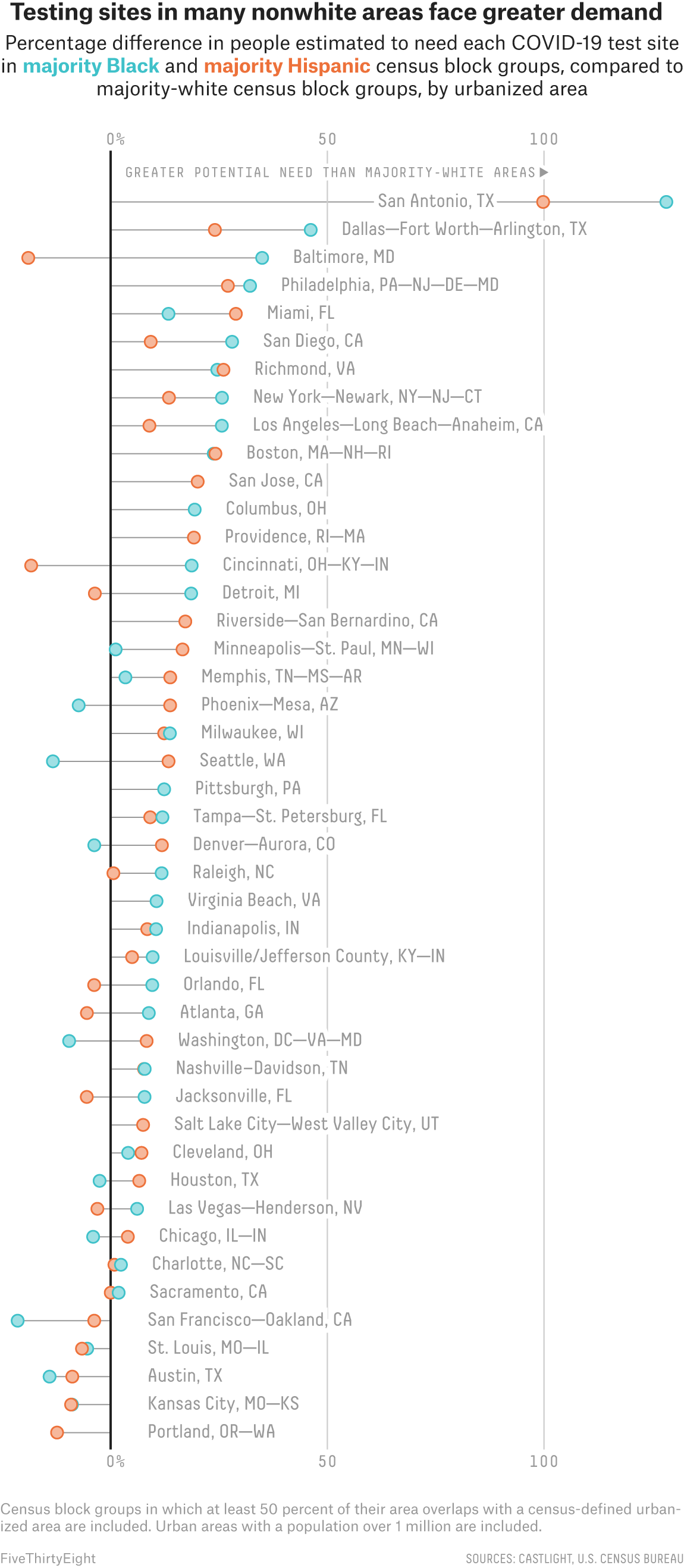
Our analysis revealed that, in many cities, testing sites in and near predominantly Black and Hispanic neighborhoods are likely to serve far more patients than those near predominantly white areas.
A similar disparity exists between richer and poorer neighborhoods, our analysis showed: Testing resources were more scarce in poorer areas, with fewer sites per person and sites located farther away. And the disparity could be even greater in real life, considering wealthier people could also get tested by private practitioners who are less likely to be reflected in our analysis.
Kevin Ahmaad Jenkins, a fellow at the University of Pennsylvania's Leonard Davis Institute of Health Economics who has been researching the impact of COVID-19 testing center availability on communities of color, told ABC News and FiveThirtyEight that his team found that testing sites serving minority communities in big cities are fewer in number, have longer lines and often run out of tests. The impact of such disparities, he said, is evident in the pandemic's disproportionate effect on people of color.
"It's just as clear as George Floyd's video. These numbers are right in front us: We are dying at disproportionate rates," he said.
The disparities we found varied in severity across the country. In some major urbanized areas, they're small or nonexistent. But in others - from Dallas to Miami to San Diego and many places in between - majority-Black and majority-Hispanic neighborhoods faced far more competition for COVID-19 testing than their white neighbors. Disparities were also seen in some predominantly Asian or Pacific Islander communities, such as those in Washington, D.C., Minneapolis and Riverside, Calif., but they weren't as widespread as those among Black and Hispanic communities.
And our calculation of potential demand for testing at some sites in those underserved neighborhoods is likely an underestimation: Based on our reporting, many of the testing sites in those neighborhoods are government-funded community sites. These sites are set up to close the gaps in testing access in different communities, but they tend to be very popular among people from all across the county or urban area because they are often free and don't require an appointment.
Accessibility in Houston
In Houston, Kenneth Hamilton, 31, waited for four hours in the line to take a COVID-19 test at Houston's NRG Stadium.
Eventually, after spotting several people not wearing masks or practicing social distancing, Hamilton - a small business owner and father of seven - decided that continuing to wait wasn't worth the risk of being exposed to coronavirus in the line itself. So he left, and looked for other testing options in his neighborhood.
But as a Black resident of Houston's Third Ward, the line Hamilton left was, at the time, his only nearby option. Three months after he first sought a test, he says there are considerably more testing centers in his neighborhood.
"One of the schools that my kids go to, and one of the schools close by in the neighborhood, and a couple of churches now have them," he said. "They ramped up, to an extent."
The Houston urbanized area is just as diverse as many other major Texas metropolitan areas, but the city's initial plans to spread testing centers out equally across its neighborhoods while still operating at capacity helped to reduce site demand.
As a result, the community demands of various neighborhoods were fairly equal. ABC News and FiveThirtyEight's analysis showed that, on average, predominantly Black Houston neighborhoods faced similar levels of potential need as white neighborhoods. Hispanic neighborhoods had slightly higher potential community need than white neighborhoods, but not by much.
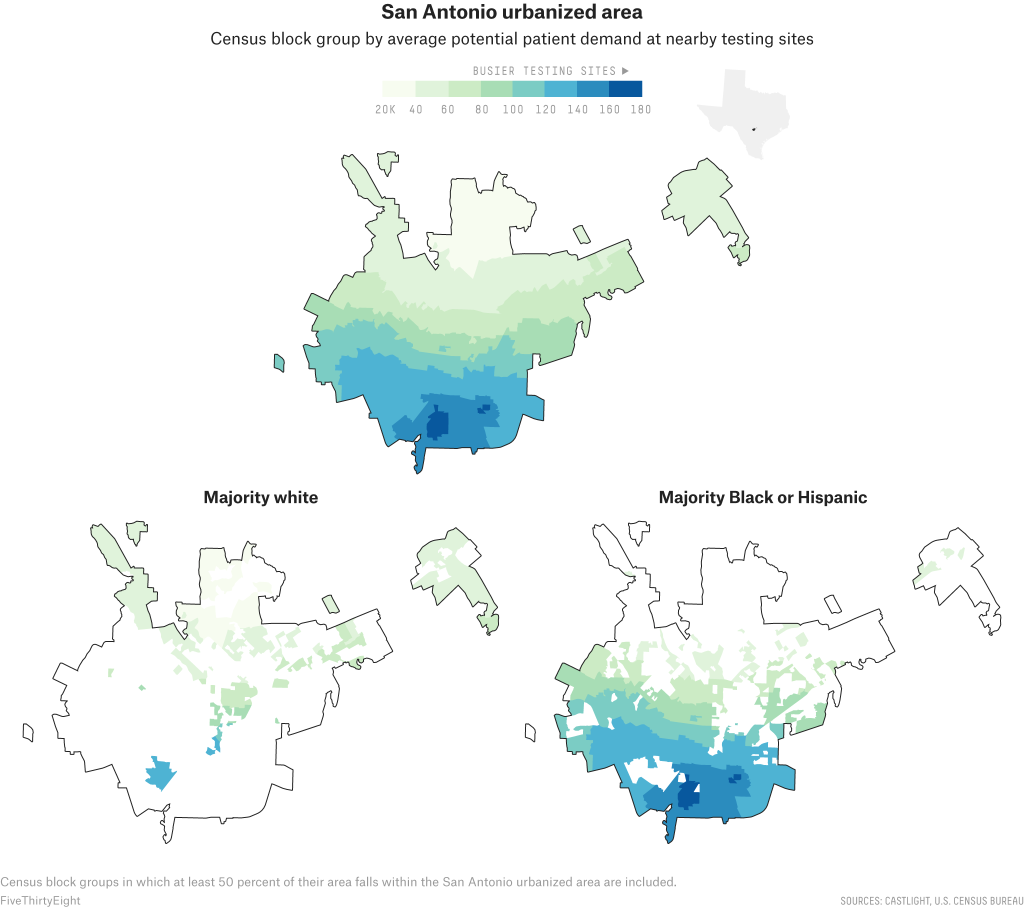
But the disparities are still clearly visible in the San Antonio and Dallas areas.
San Antonio disparities
In the San Antonio urbanized area, testing sites in poorer, majority-Black and majority-Hispanic neighborhoods in the south, east and west are estimated to have to serve far more people than sites in more affluent, whiter neighborhoods in the north, resulting in a disparity in potential community need.
According to our analysis, of the roughly 45 sites that were actively testing in San Antonio in mid-June, several sites with the lowest potential patient demand were concentrated in the northern neighborhoods of Stone Oak and The Dominion, as well as the areas surrounding Friedrich Wilderness Park, which are all majority-white communities that boast median household incomes ranging from around $100,000 to $150,000.
In comparison, many of the busiest sites are scattered in San Antonio's more densely populated downtown, where the median income ranged from just $15,000 to about $40,000.
Throughout the San Antonio urbanized area, predominantly Hispanic neighborhoods had an average potential community need twice as large as white neighborhoods; the disparity in between majority-Black and majority-white neighborhoods was even larger.
Experts say that the disparity can be attributed to a long-standing gap in the health care system and an unequal distribution of health care facilities in the San Antonio area, which is one of the most economically segregated cities in the country.
San Antonio residents are tested for COVID-19 at a free walk-up site set up by the San Antonio Fire Department.
Recognizing testing disparities in different communities, the city identified underserved neighborhoods based on its equity matrix, and put together three cost-free pop-up sites that rotate around different parts of the city every week, according to its health department.
Not only are government sites falling short of their ability to meet the public need for tests, but they themselves have become part of the disparity by concentrating demand even as they seek to address it in underserved neighborhoods. San Antonio's walk-up sites do not require a doctor's referral and, as a result, have become massively popular among those who do not otherwise have access to testing.
In late June, Jennifer Herriott, the deputy director of the San Antonio Metropolitan Health District, told us that people have lined up hours before these pop-up sites even open and that one time they had to turn down 275 people after running out of tests.
Herriott said that as the demand for testing spiked, with cases and hospitalization rates across the state setting new records on an almost daily basis, the city and the county have been working to ramp up testing capacity. The pop-up sites that used to run only three days a week now operate six days a week, and each site's capacity has been increased from about 150-200 tests per day to 350.
Still, the long lines remain in some places, and sites continue to run out of tests.
"Public health and our partnership with San Antonio Fire (Department) has consistently had its eye on making sure that we're serving our Black and brown communities," Herriott said. "As our needs increase here, we've increased free testing and those walk-ups and the Freeman drive-thru so we make sure that communities that might not be able to access testing are able to access testing."
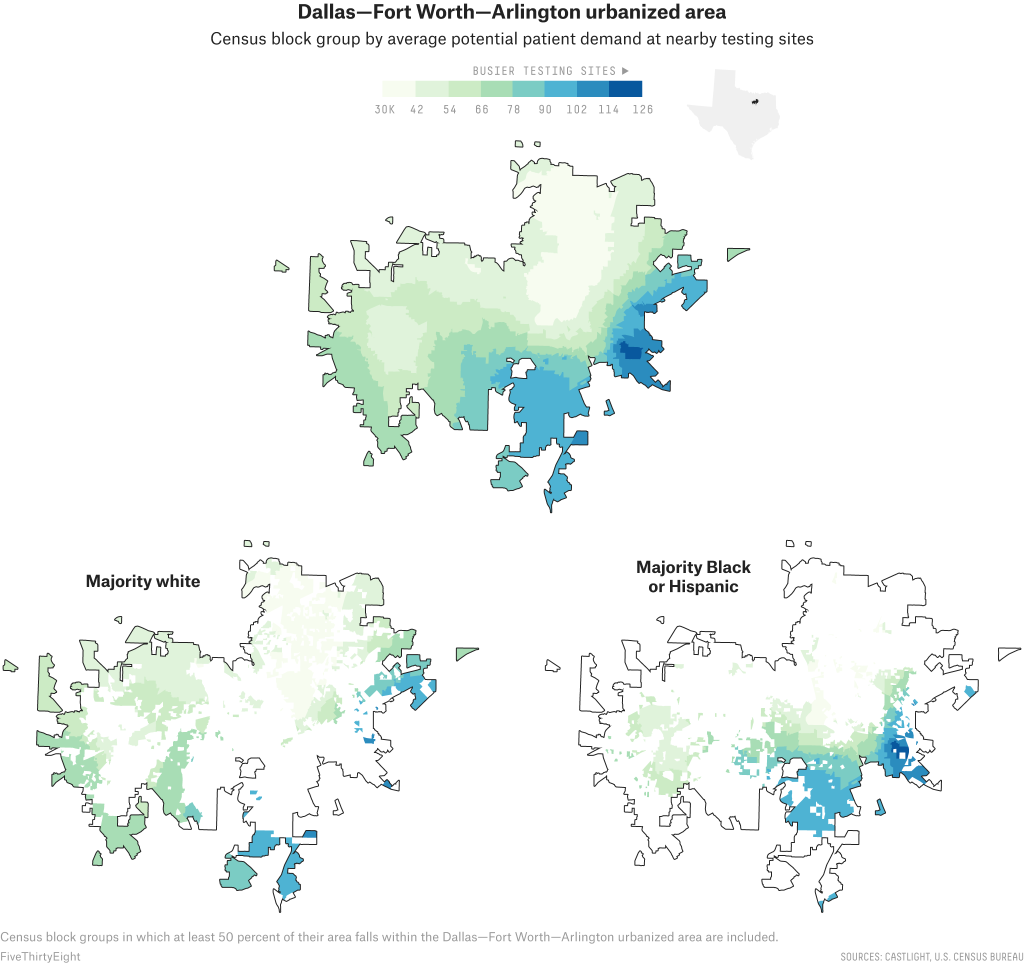
Dallas disparities
Dallas County and Tarrant County, two counties of nearly 4.7 million people that cover much of the Dallas urbanized area, have together reported over 64,000 confirmed cases of the coronavirus so far. Our data showed that in early summer, the testing infrastructure of the Dallas urbanized area - which encompasses the cities of Dallas, Fort Worth and Arlington - resembled that of San Antonio: Local and state providers, as well as private hospitals, favored people living in whiter and wealthier parts of the county, towards the north, more than those living in the less affluent areas in the south.
Across the Dallas-Fort Worth-Arlington urbanized area, our analysis found that majority-Black neighborhoods had a potential community need 46 percent higher than majority-white neighborhoods; majority-Hispanic neighborhoods had a potential need 24 percent higher.
"There's a compounding problem beyond just where the sites are," said Judge Clay Jenkins, the chief elected official in Dallas County. "The people that tend to have insurance are in the north and those that tend to not have insurance are in the south. We've planned to put the majority of our testing in places where there's high uninsured."
Take the University Park neighborhood of Dallas, where the median household income is $214,000 and almost 90 percent of the residents are white. It has at least five testing sites around the neighborhood, according to Castlight data. Appointments are required at most of them, per Castlight, which helps organize the speed at which people are able to get tested every day (walk-in testing centers tend to have longer lines).
It's a vastly different situation in Lancaster in southeast Dallas County, which has about 15,000 more residents than University Park but where Black people make up 69 percent of the population and the median household income is $53,000. Residents hoping to get a coronavirus test in the Lancaster area had to travel at least seven miles to the nearest drive-thru testing center until recently, when a nearby Walmart Supercenter opened up a drive-thru site.
To address the disparities, the city of Dallas asked the private sector to step up its support in the areas of the city most in need of more testing.
"A lot of the private providers are set up in northern Dallas, and it does highlight the existing disparities in the city," said Tristan Hallman, a spokesman for Dallas Mayor Eric Johnson. "In response, we've asked Walgreens, CVS, Kroger to locate their facilities in southern Dallas, and they've done so."
Indeed, public health experts said the issue of unequal access to testing is a direct result of long-standing decisions made by private-sector companies and entrepreneurs when selecting which neighborhoods to open new businesses in. And the disparity is exacerbated by the fact that underserved communities are less likely to have the health insurance or financial resources necessary to seek costly testing from private providers when community sites are not accessible.
"This is certainly driven by systematic health care injustice and it's actually very clearly delineated in Dallas because of gentrification and all of the social aspects of our community," said Katelyn Jetelina, a professor at the UTHealth School of Public Health in Dallas. "We need to figure out how to supplement the cost so that families in south Dallas don't have to decide whether they're having dinner or have to go get a COVID test."
Even as more testing sites have been set up in underserved communities, new coronavirus hot spots flared up over the summer as communities began to reopen; now, a lack of tests and long lines have created major problems all over the country.
Further south, along the border in Hidalgo, Texas, Isaac Garza waited 10 hours in line to get a coronavirus test after visiting several recently reopened restaurants he oversees. As he has diabetes, an underlying condition, he didn't want to take any chances, and was relieved when his test results came back negative.
But the limited testing options in his community creates problems for Garza's staff, too. Every day, Garza said, he receives calls from employees showing symptoms consistent with COVID-19 who tell him that they might have to miss critical work hours to wait in line for a test.
"It's really been challenging to do business and just to live day in and day out with all this because you're trying to protect your family, you're trying to protect your employees," he said.
Contributing: This special report is the result of a months-long investigation among three ABC news organizations - FiveThirtyEight, ABC News and ABC Owned Television Stations. In addition to reporting by ABC13, nationwide data analysis and reporting for this story was contributed by a team including Soo Rin Kim and Matthew Vann of ABC News, Laura Bronner of FiveThirtyEight and Grace Manthey of ABC Owned Television Stations. The full analysis is here and an explanation of how we did it can be found here.